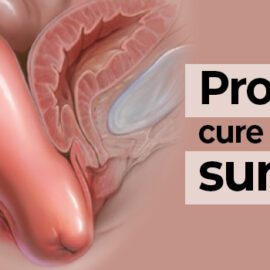
Pelvic organ prolapse, often known as prolapse, is a frequent disorder in which the bulge of the vaginal wall (drops) from its normal position. The following are the most frequent symptoms of vaginal prolapse:
- Bulging at or beyond the entrance of your vaginal canal
- Pelvic discomfort, pressure, or fullness
- Urinary incontinence
- Incomplete bladder or bowel emptying
- Vaginal blood or spotting
- Vaginal pressure
Women who have had a vaginal birth are more likely to develop prolapse, particularly if their doctor utilized devices during delivery, such as forceps (tools that resemble huge spoons) or vacuums. This is due to the fact that many women’s pelvic floor muscles atrophy after giving birth. Other prevalent causes of prolapse include:
- Age, with postmenopausal women being more susceptible;
- Connective tissue abnormalities;
- Chronic constipation or anything that produces chronically elevated abdominal pressure; and
- Family history.
Many women’s quality of life is impacted by prolapse symptoms, which make it difficult to conduct a number of daily tasks. As a consequence, if you don’t currently have prolapse, it’s critical to know what therapies are available and how to avoid it.
What Are the Treatment Options for Prolapse?
Our urogynecology team is known throughout the country for providing professional treatment to individuals suffering from prolapse and other pelvic floor diseases. Prolapse is usually treated in one of three ways:
- Keep an eye on it: Prolapse isn’t harmful in and of itself if you don’t have any symptoms. In this situation, we will prepare a care plan for you in which we will describe prolapse symptoms and request that you return to see us as soon as possible if you encounter them so that we can help you manage symptoms using the therapies given below.
- Wear a pessary: A pessary is a silicone vaginal support device that is put within the vagina and worn throughout the day. While pessaries do not address the underlying prolapse, they are non-surgical and usually alleviate prolapse symptoms. Pessaries must be removed, cleaned, and changed on a regular basis, and your doctor will fit them in the office.
- 3. Surgical intervention: In an outpatient environment, we may resuspend and correct your prolapse using a number of minimally invasive treatments. The majority of these procedures are performed via the vaginal canal, with no exterior incisions and generally without the need for general anesthesia. Other procedures are done via a “keyhole” incision. However, the precise procedure varies according to the kind of prolapse, so talk to your doctor about how the surgery would work for you and your specific case.