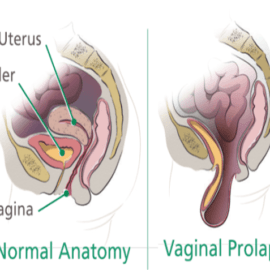
Rectal prolapse befalls when part or the whole wall of the rectum slides out of place, at times stabbing out of the anus. Patients with a rectal prolapse will normally present with rectal mucus discharge, faecal soiling, bright red blood on wiping, or even with observable ulceration. Full thickness prolapses start internally and therefore can present with a sensation of rectal fullness, tenesmus, or recurrent defecation. With time, the rectum starts to prolapse with defecation, then later with nominal coughing and straining, ultimately becoming totally external. These prolapses are chiefly susceptible to ulceration. On inspection, the prolapse might not always be evident, but can be recognized by asking the patient to strain. A digital rectal inspection is also required and an enfeebled anal sphincter is often recognized. For an alleged internal prolapse might be identified by defecating proctography and examination under anesthesia. Rectal prolapse is most common in kids and older grown-ups, particularly females.
Management and treatment
Conservative management of rectal prolapse is predominantly useful in those who do not want to undergo any surgery, with trifling symptoms, or in kids (as maximum prolapses will resolve spontaneously). Initial management takes account of enhanced dietary fiber and fluid consumption, reducing constipation and the time expended straining. Minor mucosal prolapses might be banded in clinic, although this is prone to reappearance. If we talk about the treatment choices for rectal prolapse, it is advisable to opt for herbal medicines rather than opting for the surgical methods.