How Do Doctors Diagnose Rectal Prolapse?
The symptoms of rectal prolapse consist of the feeling of a protuberance or the appearance of reddish-colored bulk that pokes outside the anus. At the start, this can befall during or after bowel movements and is a provisional condition. However, over time – owing to an ordinary expanse of standing and walking – the end of the rectum might even spread out of the anal canal instinctively, and might need to be pressed back up into the anus physically. Other indications of rectal prolapse consist of ache in the anus and rectum and bleeding from the internal lining of the rectum. These are seldom life-threatening signs. Fecal incontinence is another indication. Fecal incontinence refers to leak of mucus, blood or stool from the anus. This befalls on account of the rectum widening the anal muscle. Signs change as the rectal prolapse itself grows.
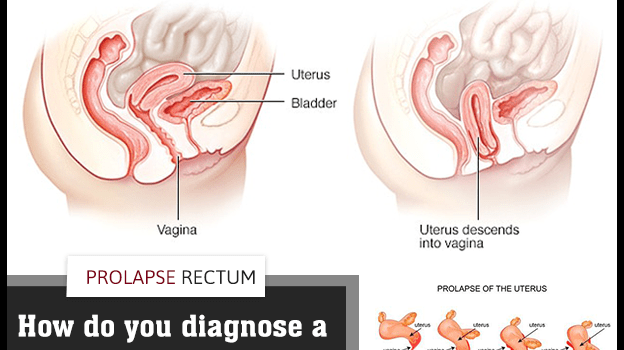
Diagnosis
During the first visit, your colon and rectal doctor will carry out an in-depth medical history and anorectal assessment. In some circumstances, a rectal prolapse might be hidden or will be internal, making diagnosis a bit more challenging. You might be asked to sit on a toilet at your doctor’s clinic and strain as if you are trying to have a bowel movement. Other examinations used for diagnosis take account of:
-
- Video defecogram: X-rays are taken while you are having a bowel movement to check muscle movement.
-
- Anorectal Manometry: Assesses muscle functions and reactions of the pelvis, rectum and anus used during bowel movements.