Full-thickness rectal prolapse must be segregated from mucosal prolapse. In mucosal prolapse, the prolapsed tissue has radial pleats at the anal junction, while a full-thickness prolapse has round pleats in the prolapsed mucosa. In mucosal prolapse, the mucous membrane alone is prolapsed and might be tangled with hemorrhoids. In complete or full-thickness prolapse, all three sheets of the rectum are prolapsed.
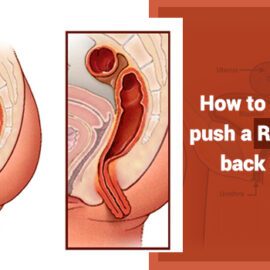
How to reduce your rectal prolapse?
Sphincter relaxation is the key to an efficacious reduction; failure is generally attributable to insufficient relaxation. Apply gentle manual pressure distally to slither the distal end of the prolapse into the lumen and via the anal sphincter. The process might take some minutes. If mucosal edema makes reduction difficult, sucrose (table sugar) might be used as an osmotic agent to decrease the edema and make reduction easier. Anecdotally, the usage of table salt has been pronounced for the same purpose. If constipation is there, it should be seriously treated. Unless infected bowel is reduced and damage results, no difficulties are predictable. A trivial amount of bleeding might happen and is not concerning.
Following prolapse, you might experience pain in the muscles surrounding the rectum i.e. the levator ani muscles. If you feel your muscles from your sitz bones, working up both sides of your butts and across just under your sacrum (the flat, somewhat rounded pad of bone at the footing of your spine) – you are feeling the levator ani muscles. There are numerous methods you can use to reduce or abolish pain in this area.