Rectal prolapse causes apprehension, fear, and discomfiture. You may feel uncomfortable speaking about your signs such as uncontainable pretentiousness and faecal incontinence. These signs can make your everyday life unhappy.
Patients identified with rectal prolapse can typically twitch treatment with a routine of workouts, diet, and medication. But the illness is advanced and may finally require surgical procedures. When a rectal prolapse influences a harshness that needs surgical interference, several specialists offer a slightly invasive option. Who Can Be Affected by This Condition?
Rectal prolapse disturbs about 2.5 of every 100,000 individuals. Females aged 50 and older are six times more possible than men to grow rectal prolapse. A weakened pelvic floor and chronic impairment also upsurge the danger of rectal prolapse.
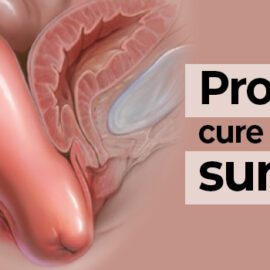
When the rectum is prolapsed and does not withdraw, it can sense as though you are sitting on a ball. Other signs include anal pain, rectal pain, faecal dissoluteness, constipation, leaking mucus, and bleeding.
- Surgery for Rectal Prolapse
The most communal surgical solution for rectal prolapse is a rectopexy. The main goals of a rectopexy process are to reinstate usual anatomy and to regenerate standard defecatory and sexual functions. A rectopexy releases the prolapsed rectum from adjacent tissues, then uses darns to secure it into location. The specialist may use mesh to sustenance and secure the rectum.
- Side Effects of Prolapse Rectum Surgery
As with any main surgery, there are some side effects involved in the process and retrieval from a surgery. Some of these risks include:
- Infection
- Constipation
- Diarrhoea
- Bowel obstruction
- Prolapse recurrence
- Pain
- Bleeding
- Damage to organs, tissues, or nerves
- Risk of fistula